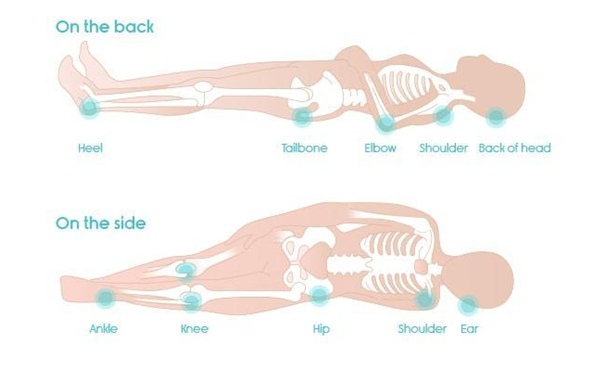
The human body and its muscles are made for movement. Most of us move around quite a lot when sleeping but oftentimes we may be confined to one position due to a severe illness, injury, or during surgery when we are under anesthesia. The lack of movement prohibits the redistribution of pressure between our bodies and the surface we lay on, creating pockets of pressure especially on those parts where the bones are most prominent. The hips, buttocks, and heels are prime spots for bedsores to develop.
How Do They Work?
What is the exact science behind this phenomenon? If the body is not moved for an extended period, the pressure caused by the body weight presses down on the capillaries that deliver blood to the skin and the underlying tissue. Due to a lack of fresh, oxygen-rich blood, the skin tissues begin to die and a red, painful bedsore starts to form.
They are a type of an open wound – providing infections an opportunity to spread to the surrounding skin, tissue, and blood. The breakdown of tissue from large bedsores can also lead to fluid and protein loss, leaving patients dehydrated and malnourished.
Bedsores are a common occurrence that the rehabilitation and recovery time is extended significantly because of bedsores developing in the initial recovery.
Can I Get One?
Staying rooted to one spot with absolutely no movement makes us highly prone to bedsores. People with any conditions that affects blood flow and its circulation are at greater risk. Such conditions include people who have diabetes or low blood pressure. For a normal person who is sleeping, shifting around in sleep is common. This is because our brains often signal us to move our bodies when they sense that too much pressure is building up at a certain spot. However, for people who are unconscious or suffering through paralysis and dementia, it is difficult for their brains to be proactive about preventing pressure buildup and bedsores.
How To Prevent One?
Keep turning your body, especially if you are tending to a bed-ridden individual. Some movement after every 2 hours goes a long way in preventing bedsores.
Make full use of support surfaces. These include mattresses and additional padding on top. As technology progresses, we now have a variety of mattresses designed to suit specific needs of patients. There are special air mattresses which alternate pressure across the entire mattress to allow movement and prevent building up-pressure on certain parts of the body. These mattresses are often used in most ICU wards as part of a standard protocol.
Do not lie down on elevated surfaces that raise your body up more than 30 degrees This should be done to avoid sliding and friction which can quicken the process of bed sore development.
Remember: Reposition yourself. If you are in-charge of an immobile patient, then move them around every two hours or so. Focus on your nutrition and skin care. Having a balanced diet and healthy skin help to slow the spread of bedsores.
